The Conundrum of PD: Are Memory Problems due to Disease, Medications or Both?: By Dr. De Leon.
The Conundrum of PD: Are Memory Problems due to Disease, Medications or Both?: By Dr. De Leon
“Understanding (PD) is like trying to put together a puzzle with pieces that don’t fit” -Dave Guerrero.
Cognitive problems and memory loss issues is one of those symptoms of PD which seem to plague all of us from day one whether we are patients or caregivers.
The thing we must first remember is that dementia is defined as loss of previously acquired skills e.g. washing dishes, cooking, driving etc. Parkinson’s dementia does not occur in typically until late stages. This means that patients would have had a diagnosis and symptoms of Parkinson’s for over 10-15 years before dementia sets in. If anyone has symptoms of dementia present earlier than this than chances are the disease they have is not typical, common garden variety Parkinson’s but a variant which could include things like PD plus syndromes (MSA, CBGD, LBD) or another dementia disorder such as FTD or Alzheimer’s and PD as well as other neurological diseases that can have parkinsonism, like strokes. Having said this, all patients notice a change in their cognition from the very beginning of the disease even before motor symptoms are noticeable.
Does this mean there is dementia? No!
The usual symptoms I am referring to that patients commonly experience are related to personality such as getting more irritable, short tempered, anxious and depressed. Sometimes, we as patients may not realize these subtle changes like increase impatience; but those close to us notice and may call it to our attention or become aware of these changes before we do. At the onset of my PD, I began to notice increased irritability and frustration especially when working at the office which I could not understand since I was the queen of multitasking. I was NOT alone in my perception my staff of many years also noticed a change in my personality that was out of character for me and something was wrong! Fortunately, this symptom improves with treatment. But, is one of the first signs of PD in most people and if not careful can go untreated for years.
Second, all Parkinson’s medications can cause cognitive changes usually in the form of brain fogginess, sedation, trouble with word finding, and depression which can cause forgetfulness. This is why is imperative to make only one medication change at a time and follow up with your doctor shortly after every new medication change to evaluate outcome and most importantly tolerability. Be on the lookout for cognitive problems due to medications, these symptoms will come on within a week of staring new medicine typically and will aggravate or worsen after each dose intake within a few hours and last as long as medication Effect lasts. This is why it is important to pay attention to medicines and a keep chart of times and effects of all medicines and talk to your doctor if you notice cognitive changes. But be sure, not make changes or discontinue regimen without first discussing with your physician.
Third, because PD usually affects mood as in depression as well as sleep, as in restless leg (RLS), sleep apnea, REM behavior, these if not properly treated can by themselves cause memory loss usually in the form of poor concentration which leads to short term memory loss because one cannot encode information into long term when not paying attention due to being tired, sleepy or fatigued, plus it is through deep sleep that our brain processes all information and makes long term memories.
Fourth, just as our bodies become slow so do our brains in retrieving information, pulling and opening the file cabinets where information is stored can be difficult. It does not mean is lost simply means that takes a little longer. Solution increasing dopa and mental exercises-
Fifth, however after a number of years as PD advances, up to 50 % of patients have a chance of developing PD dementia which is characterized by psychiatric tones like delusions, psychosis, hallucinations (visual) along with apathy and pronounced forgetfulness. Treat with Acadia; anticholinesterase (e.g. Aricept, Exelon); Provigil (among other stimulants); Namenda as well as antipsychotics (Clozaril).
In my experience as a Parkinson’s doctor, patient, and caregiver the overwhelming problems with memory in the majority of PD patients, unless they are end -stage disease beginning to hallucinate becoming apathetic which are signs of early dementia setting in, are a combination of Parkinson’s disease itself as well as medication (usually not enough). The result of insufficient dopa in the brain as well as not properly treating and addressing non- motor symptoms which interfere with concentration is poor memory. Thus, long term memory appears impaired because the majority of PD patients are sleepy, depressed, under- and- over -medicated, as well as fatigued. Early recognition of all non- motor symptoms of PD which includes side effects of medications as well as early detection of PD dementia is key, after all even the hardest puzzles have a solution.
Finally, I recommend every patient have a baseline MMSE (mini mental status exam) or Mocha test followed by every year unless symptoms of forgetfulness and apathy or other sings of forgetfulness arise. If depression is significant and can’t tell if memory problems are due to depression or early onset of dementia recommend Neuropsychiatric evaluation. If a person has profound depression unresponsive to meds consider ECT (electroconvulsive therapy) which works great.
The basic understanding of the various puzzle pieces which make up memory and cognitive changes in PD along with the correct treatment will lead to improved quality of life along with decrease chances for nursing home placement or prolonged hospitalizations.
Loss of Smell in PD: by Dr. De Leon
Loss of Smell in PD: by Dr. De Leon
“Smell is a potent wizard that transports you across thousands of miles and all the years you have lived.” -Helen Keller
Imagine not being able to smell your favorite food, perfume, or flower in my case the star-gazer lily. Smell is intricately connected to our memories. Have you ever walked into a place and immediately transported to a bye gone era simply by an aroma?
Smell is a huge component of our everyday life, as I first discovered as an undergraduate when we did an experiment in which we were asked to drink of a substance while holding our nose tightly….after sipping the clear substance, we all unanimously hailed it as water. But after, the professor asked for us to drink the same liquid without holding our nose our astonishment was evident—-it was LEMONADE! A simple pinching of our nose had altered our perception of the world!
Loss of smell can be one of the earliest signs of Parkinson’s disease. It is believed that the olfactory bulb impairment is due to clumping of alpha synuclein…. (a normal protein found abundantly throughout the brain and in smaller amounts in heart, muscles and other tissues- believed to be an important player in maintaining synaptic vesicles in pre-synaptic terminals- these are the ones responsible for release of neurotransmitters like dopamine).
Recent data suggests that >95% of Parkinson’s patients present with significant loss of smell. This may be supportive of new theory that Parkinson’s disease starts in the olfactory bulb and not in basal ganglia as previously believed.
Besides helping us with survival by avoiding harmful substances like toxic gases or rotten foods the olfactory system help us to maintain personal hygiene, which allows us to interact with others socially.
Loss of smell has been linked to cognitive decline and loss because of that primitive connection to our memory banks; therefore it should come as no surprise that this is a harbinger of dementia –olfactory loss being one of the first symptoms and signs of Alzheimer’s and PD. Loss of smell has also been linked to psychiatric problems such as depression another common symptom of PD.
However, most people don’t really notice a loss of smell per say but rather a loss or change in taste because as I mentioned earlier taste is directly linked to our ability to smell. So food begins tasting bland and sometimes even foul. But when formerly tested using a Snell smell test, PD patients show deficits in discrimination, detection, and identification of odors.
At this time there is no known cure for hyposmia (decrease ability to smell) or anosmia (complete loss of smell or inability to smell). Smell problems are often overlooked in the medical community since they are not deemed critical to living yet they have a great impact upon our lives as I stated before. Much research is needed in this field particularly if it has potential to alter our moods and cognition.
However, the best we can do is try to augment gustatory strategies and be cognizant of potential hazards and install protective measures such as fire alarms- since smoke may not be detected. Make sure inspect expiration dates of food carefully. Simulated odors are available to use while cooking for those of us who cannot smell to increase sensation of flavor. However, these odors are quiet pungent to normal smelling people so would not advice using if there are people who have normal smell in family.
Other ways to circumvent this is by enhancing gustatory senses via creative cooking such as preparing and eating foods which are spicy, crunchy, and full of aromatic herbs, as well as adding color and textures to your foods in order to engage your other senses like sight and make your whole mouth titillate and vibrate with joy….. Bon Appetite!
Source:
Freezing Gait in PD: By Dr. De Leon
Causes & Treatments for Freezing Gait in PD: By Dr. De Leon
am a slow walker but I never walk backwards. Those who walk with God ALWAYS reach their destination.”- Unknown
When I first began having symptoms of PD I was falling often because I was tripping on my left foot which would get stuck on the floor rather than continue stride – more often while initiating stride. Over the years my symptoms improved with treatments both medical and ancillary. However, at each progression of disease stage there is always a tendency to have more difficulty ambulating particularly in small confines.
Freezing is a condition seen in Parkinson’s disease which in my experience can involve one or both lower limbs. The degree of freezing worsens over time as disease progresses. However, the pattern of gait is changed from the early onset of disease this is why so many of us fall and trip on our feet early on in the disease. This by far has been one of the most difficult things to treat with an estimated 30% of individuals with PD having significant difficult with this. However, I think that part of the reason for this inability to treat is poor understanding of what is going on mechanically as well as sensory- visual.
Freezing which is described as inability to pick up the feet making them feel like they are stuck to the ground. It occurs more often at the initiation of gait especially when arising from a sitting position worse if you have been sitting for prolonged periods of time in a tight space or low chair in my experience. Also occurs early morning with – morning offs and when medicine is wearing off.
Risk factors for developing freezing of gait are absence of tremor (early on in the disease) and PD beginning as a gait disorder. The development of freezing of gait in the course of the illness is strongly associated with the development of balance and speech problems, less so with the worsening of bradykinesia, and is not associated with the progression of rigidity. Less likely to have this problem if you are tremor dominant.
Triggers for freezing are usually visual in nature in my opinion and in my personal experience- they present more commonly in dim places, crowed halls or rooms, when there is a sudden change in direction especially in corners but when there is a contrast problem in visual perception that obscures exact depth of walk ways it tends to cause freezing and hesitation because I believe our brain is trying to decide whether is safe to walk or not. Really trying to avoid falling. However, because we are slow and also have shift in gravity forward our bodies are not often able to compensate or adjust readily to this new data input from our brain causing us to fall.
Some of the things that are associated with freezing or that appear to worsen this phenomena is anxiety- which in my experience is seen when medication is off or poorly controlled motor symptoms which stand to reason that if our motor function is less than optimal we will not be able to ambulate optimally.
Each time I have fallen in the past few months has been an indicator of need to adjust medications. Each time with increase levodopa dose my symptoms have improved.
However, for reasons unknown Mao inhibitors such as eldepryl, depranyl, zelpar, azilect are particularly good at improving balance – I personally believe that each patient particularly when levodopa adjustment is not sufficient to prevent freezing should use these medications. Interestingly – in my experience these medicines especially azilect are quite good at improving visual deficits and problems with contrast which reaffirms to me at least at some degree that visual sensory loss has lots to do with freezing. The new medication xadago which is also mao inhibitor in part did not seem in my case help with this issues I was on for a month at maximum dose – perhaps over longer period of time this would help. But the other maoi’s in my experience have had direct benefit on visual problems and freezing gait within a week of initiating. Interestingly, there was a small study that indicated that Aricept is another good drug for treatment of gait freezing – since this drug directly improves not just motor executive function but also how sensory information is processed in the brain it would make sense that improvement in visual information processing would improve gait issues.
How do we treat?
The main thing is to first discover whether this pattern of walking or lack thereof is related to an “off” state and time of day. Is there anxiety at the time? Is it happening at night or poorly dimmed corridors, hallways or crowed areas? Does it happen after sitting long time or when arising from cramped conditions like being on a plane long time or sitting on a low chair couch?
Make sure that home is well lit, hallways and corridors are wide, remove carpets which can cause friction, make sure vision is corrected, build open spaces in your home, get chairs that can lift up when sitting, stand for a few seconds before initiating walk. Use assistive devices when needed, try not to sit for long periods of time without moving/stretching, and adjust medications frequently! Engage in PT, OT, exercises for balance such as yoga, tai-chi, walking on sand and deep water exercises.
I guarantee that if we follow these rules our freezing gaits will certainly improve. Avoid shoes with traction.
Sources:
http://movementdisorders.ufhealth.org/2011/11/23/physical-therapy-tips-for-freezing-of-gait/
http://www.epda.eu.com/en/parkinsons/in-depth/pdsymptoms/freezing/
Freezing of gait in PDN. Giladi, M. P. McDermott, S. Fahn, S. Przedborski, J. Jankovic, M. Stern, C. Tanner, The Parkinson Study Group Neurology Jun 2001, 56 (12) 1712-1721; DOI: 10.1212/WNL.56.12.1712

@copyright2019
all rights reserved by Maria De Leon MD
THE CHANGING FACE OF PARKINSON’S DISEASE : By Dr. De Leon
THE CHANGING FACE OF PARKINSON’S DISEASE : By Dr. De Leon
“Your spark can become a flame and change everything!”- E.D. Nixon
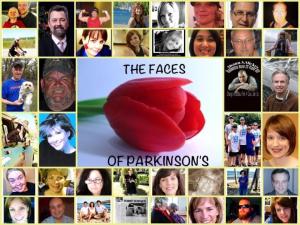 As we commemorate one more year of Dr. Parkinson’s Birthday, we are reminded of the great accomplishments in the area of PD and neuroscience since he was a prominent physician in London. Yet, human kind has been battling a form of ‘Parkinson’s’, if not the same illness, for centuries before Dr. Charcot put a name to it in honor of James, dating back to the times of ancient India. From history we know that this disease does not discriminate against race, ethnicity, or social economic status. Currently, it is believed that there are approximately 10 million people world-wide suffering from this disease.
As we commemorate one more year of Dr. Parkinson’s Birthday, we are reminded of the great accomplishments in the area of PD and neuroscience since he was a prominent physician in London. Yet, human kind has been battling a form of ‘Parkinson’s’, if not the same illness, for centuries before Dr. Charcot put a name to it in honor of James, dating back to the times of ancient India. From history we know that this disease does not discriminate against race, ethnicity, or social economic status. Currently, it is believed that there are approximately 10 million people world-wide suffering from this disease.
We have learned, however, that although mostly sporadic in nature there are some genetic predispositions to developing Parkinson’s disease which vary from one family to another and from one ethnic group to another. Despite the genetic predisposition it seems that environment and outer influences such as exposure to toxins can hasten the development of this illness in an otherwise normal individual.
Here are the most common Risk factors:
- Advancing age
- Male gender
- Decrease estrogen /early hysterectomy with ovary removal
- Environmental toxins
- Low Folate levels
- Agricultural workers
- Well water consumption
- History of essential tremors increases -depending on who you quote there is a 10-30% increase
- History of melanoma
- History of chronic constipation
- History of mood disorders
- History of sleep disorders such as RLS/REM behavior
- Repeated head trauma or severe head injury
- Family history of PD
- Ethnicity- Hispanics twice as likely to develop
- Occupation- those in medical field are also at greater risk presumably due to exposure of toxins and stress since the basal ganglia is overly sensitive to stress-may trigger faster aging process in the basal ganglia
Change is an inevitable part of life, without change there cannot be growth. The truth is that we are now in the middle of the PD pendulum swinging back. Since the name of Parkinson’s was ascribed to a disease that affects our motor system, causing slowness of movement, along with gait difficulty, rigidity of muscles and rest tremors that dissipate in sleep and when engaged in purposeful movement, was thought that PD was a disease of middle to late age white men. No longer is it just a “movement” disease but an entire body system illness affecting our thinking, our personalities, and almost every system from head to toe excluding the lungs. Now it also appears that PD is encompassing a much younger population many of whom appear to be women. So, no longer are the young and ‘fairer’ sex protected but rather caught up in the midst of the storm.
Therefore, it is up to all of us to do what ever we can big or small in fight against PD. We can volunteer for research studies, write our congressmen http://www.parkinsonsaction.org about needing more doctors and funding to provide for day to day issues encountered by those of us who live with PD in our lives either as patients or caregivers. we can offer our services to help those with PD, we can donate our monies to PD foundations such as http://www.pdf.org , you can purchase a ‘Parky Raccoon’ to help send someone to WPC next year or simply to raise awareness for a still obscure disease in many circles.